Case of the Month by Morgane Dubois
CLINICAL PRESENTATION
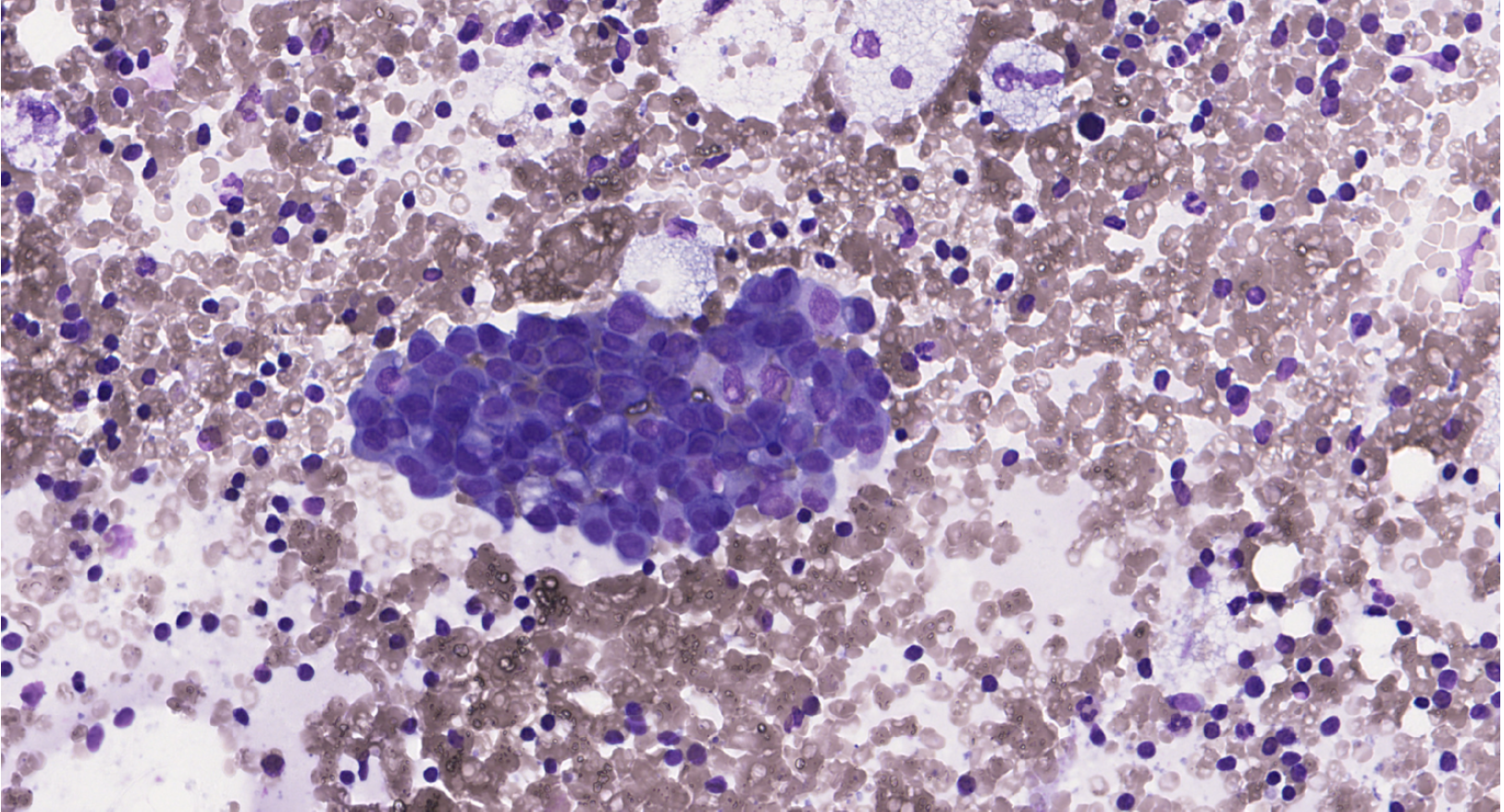
This is a 77-year-old woman with a 10-mm BI-RADS 4 mass in the upper inner quadrant of
the left breast. Core needle biopsy shows invasive carcinoma of no special type (NST),
Nottingham grade II (Elston–Ellis). Hormone receptors positive (100%), HER2 1+, Ki-67
20%. Homolateral axillary lymph node ultrasound demonstrates cortical thickening to 4
mm. An ultrasound-guided fine-needle aspiration of the atypical lymph node was performed.
Two direct smears were prepared and stained with MGG.